What Is Female Incontinence, And Best Ways To Manage It
Female incontinence, or the reduced control of bladder or bowel habit, may seem like an uncomfortable topic to talk about, yet it’s a common issue affecting every 1 in 3 women. As such, it’s important for us to understand the different types of incontinence, and what we can do to manage this condition.
Pelvic Floor Muscles
In order for us to understand the condition, we must first understand the functions of our pelvic floor muscles, which control excretion from the body through urination and passing bowel movements.
Pelvic floor muscles are muscles that help to stabilise the pelvis and spine, as well as support and protect the function of our pelvic organs like the bladder, uterus, and rectum. They also assist with sexual function and childbirth.
Incontinence
Prolonged underuse or overuse of pelvic floor muscles can cause their weakness, meaning that the pelvic organs are not well supported to perform their designated functions. The resulting condition is called incontinence, i.e. reduced control of bladder and bowel movements.
Incontinence can have many stages, from leakage of small volumes, to full inability to inhibit the passing of urine or stool from the body. For this reason, the symptoms tend to be often overlooked.
1. Stress Incontinence
Stress incontinence occurs when the intra-abdominal pressure (pressure between the abdomen and the pelvic floor) is increased and excess pressure is placed on the pelvic floor. The pelvic floor cannot resist against this pressure effectively, and due to the pressure’s strength, the muscles are unable to maintain the body’s continence.
This often leads to a leak of urine, especially during activities such as excessive coughing, sneezing, laughing, running, jumping, and lifting weighted objects.
2. Urge Incontinence
Urge incontinence occurs when a person is unable to hold or control their bladder due to training the bladder incorrectly, such as going to the toilet too frequently when the bladder isn’t full.
The bladder can hold up to 500mls of urine, but we get the initial urge to empty it at just 200mls. However, consistently emptying it at this level can lead to a shrinking of the bladder and subsequent inability to hold urine in. Research shows that we should only be making 4-6 visits to the toilet, per day (subject to fluid intake and activity level).
However, it is not good to hold it in too long, either! Not urinating frequently enough can lead to overstretching of the bladder, weakening it and causing voluntary contraction at a later stage (leakage or incontinence).
3. Mixed Incontinence
Mixed incontinence is a mixture of stress and urge incontinence as it shares common symptoms of both. There is a variety of causes for this condition:
- Hereditary – (eg. giggle incontinence which occurs when laughing)
- Chronic history of constipation (e.g. excessive pushing that leads to overusing the pelvic floor muscles)
- Trauma to the pelvic floor (e.g. tears or episiotomies following labour)
- Weight training (e.g. struggling to lift heavy weights, causing our pelvic floor muscles to compensate and take additional pressure)
- Hormone changes in menopause
- History of haemorrhoids
- Longer duration of labour or time of pushing
- Increased number of vaginal deliveries
4. Incontinence Caused by Prolapse
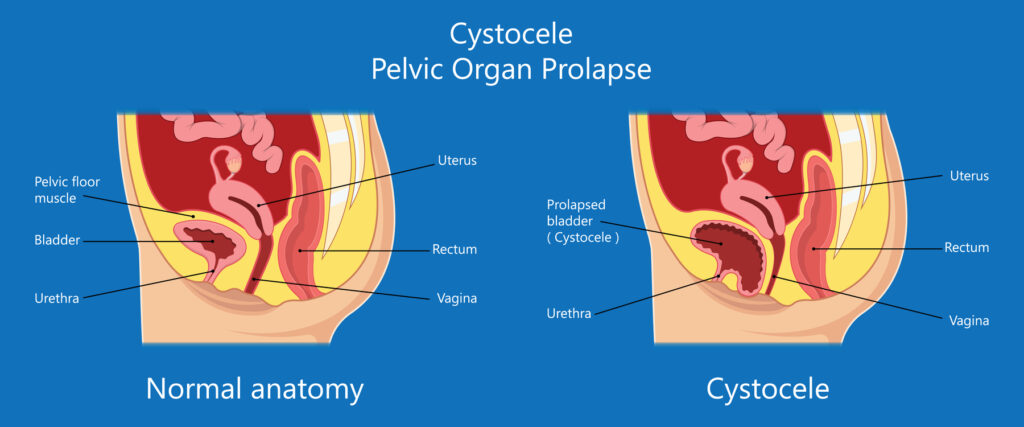
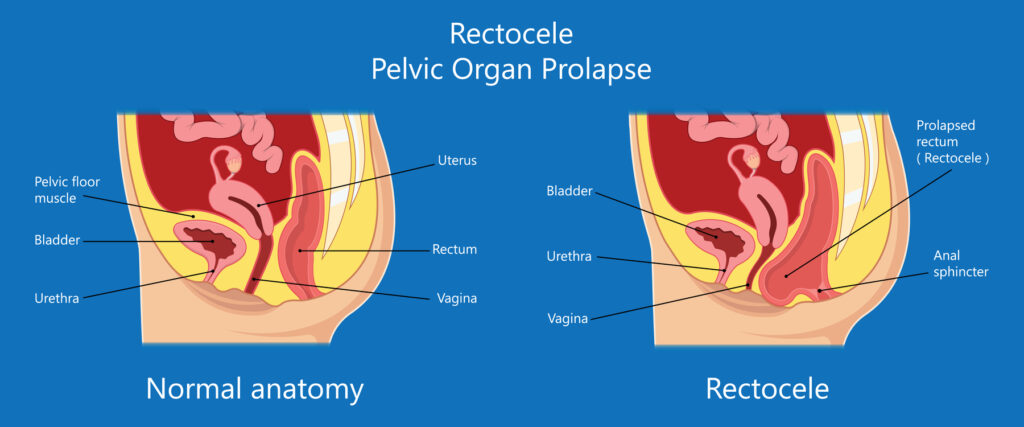
A prolapse occurs when the anatomy of the bladder, vagina walls and cervix is altered due to a weakness and hence, a lack of support from the pelvic floor. A prolapse may cause either incontinence or difficulty in passing urine or motion fully. There are 2 types of prolapse, cystocele and rectocele.
Cystocele is a weakness of the anterior wall of the vagina, a condition in which the wall does not stand upright and isn’t as strong as it should be, creating a curve or bulge.
- If the cystocele is higher up on the anterior wall, it can rest on the bladder, causing irritation and leakage of urine.
- If the cystocele lies further down the wall, urine can accumulate in this pocket and therefore result in incomplete emptying of urine from the body.
Rectocele is a bulge in either the posterior wall of the vagina or anterior wall of the rectum. This can lead to difficulty in having a complete bowel movement as parts of the stool may enter the ‘pocket’ that is formed within the wall.
People suffering from a rectocele will typically place external pressure to the perineum to straighten the curve and facilitate complete movement.
Although our anatomy may not return to its original position, there are a number of ways to improve these symptoms so that our daily lives are not impacted.
Best Ways To Reduce Incontinence
Tip #1: Reduce Your Caffeine Intake
Coffee, tea, and fizzy drinks all contain caffeine. Try to avoid or limit your intake of these as well as acidic juices, as they may all irritate your bladder. Despite popular belief, green tea actually consists of more caffeine than normal tea bags.
Bonus tip: Always use another mug to first dip your teabag into hot water as it removes 70% of the caffeine. This reduces the caffeine concentration in your drink.
Tip #2: Squatty Potty
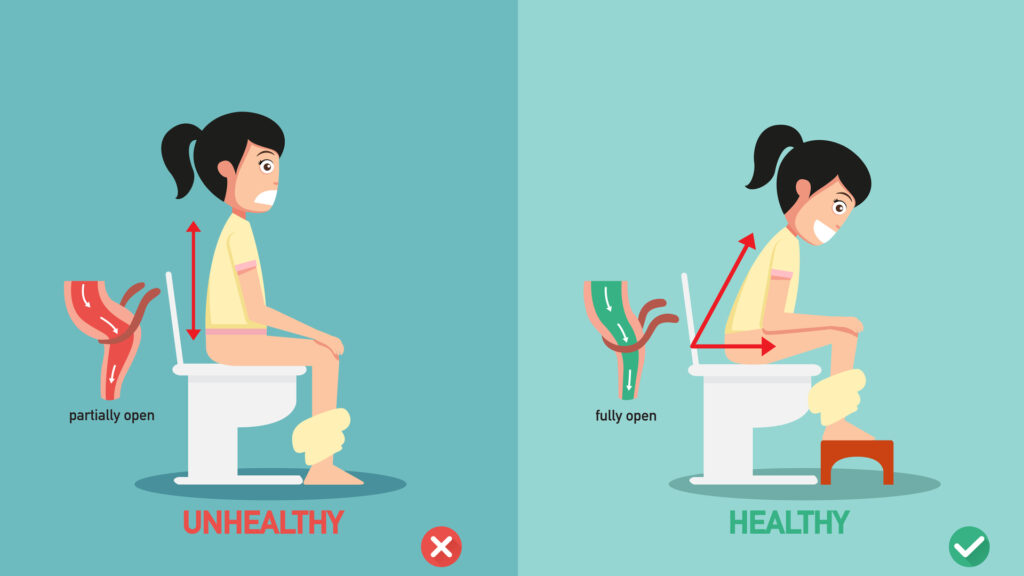
Did you know that our bodies were designed to squat when we open our bowels?
The intestines within your bowel are controlled by the muscles surrounding them. The area where the rectum meets the anal canal (as pictured below), a muscle called puborectalis, loops around the outside. When it contracts (in a normal sitting position), it causes the angle between the rectum and the anal canal (the anorectal angle) to bend to approximately at 90 degrees – preventing faeces from exiting the body.
If the angle is increased to 180 degrees, the stool can descend easily towards the anus. Here is how you can adapt your sitting posture on the toilet:
Relax your abdominals. Instead of holding your breath and tightening your stomach, stick your stomach out and bring your legs up towards you (squat). You can place a small child’s step or box underneath your feet to avoid straining.
Tip #3: Love Your Pelvic Floor
People often ignore pelvic floor exercises, thinking ‘it’s just a little exercise for a small part of the body, which won’t make much of a difference’. WRONG!
As mentioned, everyone uses their pelvic floor muscles throughout the day without even realising it. It has been proven that strengthening a muscle before it goes through trauma, like an operation or labour, will make it stronger afterwards. Strengthening your pelvic floor is essential for all women, with or without symptoms.
Follow these steps to train your pelvic floor muscles:
- Squeeze your back passage, as if to stop yourself from passing wind
- Tighten the back, and lift the front upwards and forwards as if pulling your pelvic floor towards the front of the body
- Do not contract your glute muscles or abdominals
- Keep breathing!
See how many seconds you can hold the contraction before it eases off. Fast-twitch muscle fibres are activated with repetitive small contractions of this exercise, which will help to train your endurance fibres of your pelvic floor.
How Physiotherapy Can Help
If you think you’re suffering from incontinence, don’t worry – there are different ways to address it! For example, Women’s Health Physiotherapists are professionals who specialise in this area and are able to assist you with expert advice and step-by-step treatment.
Reach out to us here to make an appointment.
Written By: Kate McCormack – B.Sc. (Hons) Physiotherapy (UK)
Kate is an experienced Physiotherapist specialising in musculoskeletal physiotherapy with a special interest in women’s health. She is skilled in treating post-natal injuries, including post-labour tears and haematomas, episiotomies, pain, and tight pelvic floor muscles. She is also trained in assessing and treating incontinence resulting from stress on the pelvic floor, overactive bladder and prolapse, for women of all ages.